Substance Abuse and Mental Health Dental CE Strategies
Substance abuse and mental health dental CE is gaining attention as dental professionals increasingly encounter patients with behavioral health issues. As the link between oral health and mental wellness becomes clearer, continuing education (CE) is evolving to equip dentists and hygienists with crucial interdisciplinary skills. This article explores how substance abuse and mental health intersect in dental care, and how CE programs can help dental professionals respond effectively.
Understanding the Fundamentals
Before exploring advanced strategies, it’s essential to understand the core concepts of substance abuse and mental health in the context of dental care. These issues are not just medical or psychological—they have significant oral health implications.
The integration of behavioral health into dental CE is a response to rising cases of addiction and mental illness affecting dental outcomes. Many dental professionals report feeling underprepared to deal with these issues due to traditional training gaps.
1.1 The Oral-Systemic Connection
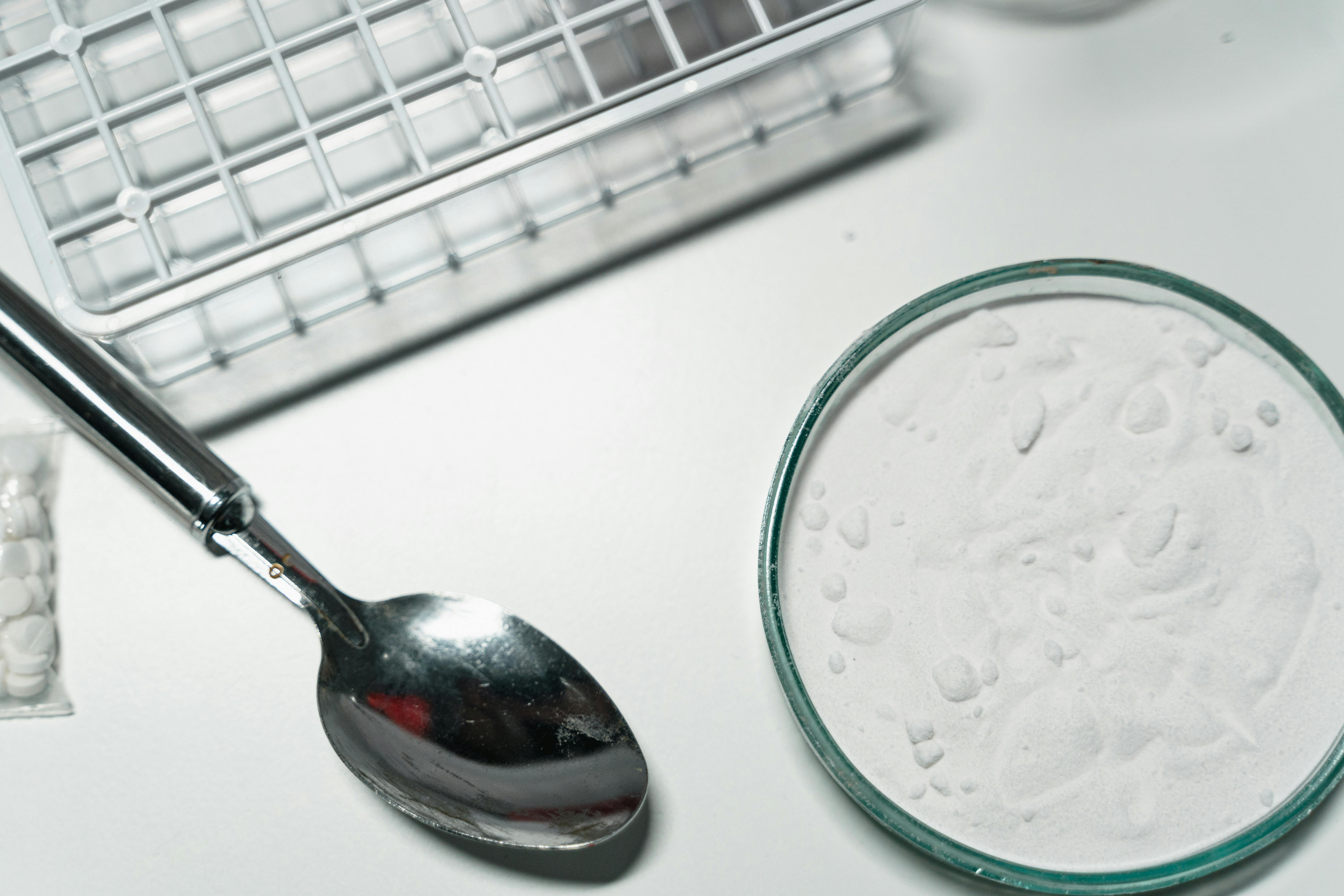
The connection between oral health and systemic health has long been acknowledged. For example, chronic drug use can lead to rampant caries, periodontal disease, and tooth loss. Mental illnesses like depression often result in poor oral hygiene practices, contributing to a cycle of neglect.
According to the National Institute of Dental and Craniofacial Research, individuals with mental illness are 2.7 times more likely to lose all their teeth than those without. This underscores the need for targeted CE programs in this area.
1.2 Behavioral Risk Factors
Behavioral factors such as poor nutrition, tobacco use, and neglect of oral hygiene are common among patients struggling with mental health or substance use disorders. Unlike other risk factors, these are influenced by psychological states and socioeconomic environments.
Dental CE that addresses behavior modification techniques can empower clinicians to intervene early. Programs that include motivational interviewing and trauma-informed care show promising results in improving patient outcomes.
Practical Implementation Guide
Applying what is learned in CE courses to real-world practice can be challenging. However, structured approaches can ease this transition and improve patient engagement and outcomes.

2.1 Actionable Steps
- Assessment and Screening: Implement mental health and substance use screenings as part of initial intake forms. Include questions on sleep, anxiety, alcohol, and drug use.
- Resource Integration: Establish referral networks with mental health providers. Include these resources in patient education materials.
- Staff Training: Offer internal training sessions or CE workshops focused on recognizing behavioral health issues and applying compassionate communication techniques.
2.2 Overcoming Challenges
Dental professionals often face obstacles such as time constraints, stigma, and lack of training when addressing mental health or substance abuse. Here are a few common issues and solutions:
- Time Limitations: Incorporate behavioral health discussions into hygiene appointments or treatment planning sessions.
- Patient Resistance: Use motivational interviewing to build trust and encourage open dialogue.
- Knowledge Gaps: Leverage online CE platforms to stay updated without disrupting practice hours.
Monitoring for red flags like unexplained weight loss, rapid dental deterioration, or erratic behavior can help clinicians detect issues early. Experts also recommend documenting all observations and interventions carefully.
Advanced Applications
Once foundational knowledge is applied successfully, dental teams can adopt more advanced strategies to integrate behavioral health into long-term care planning. These methods offer comprehensive solutions for high-risk patients.

3.1 Multidisciplinary Collaboration
Working with psychologists, addiction counselors, and social workers enhances treatment effectiveness. Case studies show that interdisciplinary teams significantly reduce relapse rates and improve adherence to oral care regimens.
In one California-based program, patients receiving coordinated behavioral and dental care reported 40% fewer missed appointments and improved treatment outcomes over a 6-month period.
3.2 Digital Health Integration
Telehealth and digital record-sharing systems streamline communication between dental offices and behavioral health providers. These platforms allow for better continuity of care and real-time updates on patient progress.
Practices must ensure HIPAA compliance and proper consent protocols, but once in place, these technologies foster seamless care coordination and reduce duplication of services.
Future Outlook
The next wave of innovation in dental CE is expected to focus more heavily on behavioral health competencies. AI-driven diagnostics, virtual CE simulations, and augmented reality tools may play key roles.
By 2030, the American Dental Association predicts that behavioral health training will become a standard requirement for licensure renewal. Preparing for these changes now ensures long-term adaptability and professional growth.
Conclusion
In summary, substance abuse and mental health dental CE is not a luxury—it is a necessity. Key takeaways include understanding the oral-systemic connection, implementing practical tools, and pursuing advanced interdisciplinary approaches.
Dental professionals should explore accredited CE options that address behavioral health, implement screening protocols, and establish community partnerships. Investing in this training will elevate the standard of care for vulnerable populations.
Frequently Asked Questions
- Q: What is substance abuse and mental health dental CE? It refers to continuing education courses that train dental professionals to manage patients with mental health or substance use challenges effectively.
- Q: How do I get started with these CE programs? Look for ADA-approved or state-licensed courses that include behavioral health modules and hands-on case studies.
- Q: How much time does it take to complete these courses? Most range from 4 to 20 hours depending on the format—live seminars, online modules, or hybrid models.
- Q: Are these courses expensive? Costs vary, typically between $50 to $500, depending on provider and depth. Many offer group or early registration discounts.
- Q: How does it compare to standard dental CE? These programs offer specialized knowledge not covered in general CE, making them ideal for patient-focused practices.
- Q: Is this type of CE difficult? While it requires a learning curve, especially in communication and psychology, most professionals find it manageable and highly rewarding.
- Q: Can this apply to pediatric or geriatric dentistry? Absolutely—children with developmental disorders and seniors with cognitive decline both benefit from providers trained in behavioral health care.
